Nursing diagnosis increased intracranial pressure delves into the intricate complexities of a critical condition, providing a comprehensive exploration of its pathophysiology, clinical manifestations, nursing management, and collaborative care. This discourse unveils the crucial role of nurses in recognizing, assessing, and intervening to mitigate the potentially devastating effects of elevated intracranial pressure, emphasizing the significance of interdisciplinary collaboration and patient education.
As we embark on this journey, we will dissect the underlying mechanisms leading to increased intracranial pressure, unravel the clinical signs and symptoms that herald its presence, and delve into the evidence-based nursing interventions employed to manage this delicate condition.
Furthermore, we will elucidate the collaborative efforts of healthcare professionals and the indispensable role of patient and family education in optimizing outcomes.
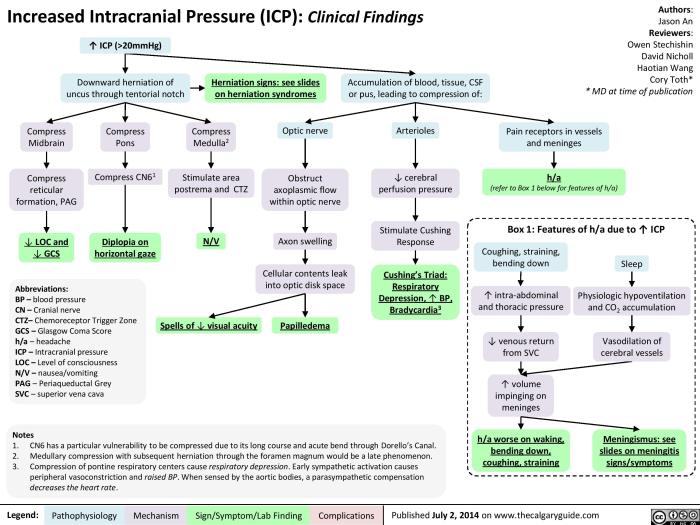
Pathophysiology of Increased Intracranial Pressure
Increased intracranial pressure (ICP) occurs when the pressure within the cranial vault rises above normal levels. This can be caused by a variety of factors, including:
- Increased intracranial volume, such as from a brain tumor or hemorrhage
- Decreased intracranial compliance, such as from a skull fracture or infection
- Obstruction of cerebrospinal fluid (CSF) flow, such as from a hydrocephalus
The Monro-Kellie doctrine states that the volume of the intracranial contents is constant. This means that an increase in one component (such as brain tissue) must be compensated for by a decrease in another component (such as CSF or blood).
When the compensatory mechanisms are overwhelmed, ICP increases.
Increased ICP can lead to a variety of symptoms, including:
- Headache
- Nausea and vomiting
- Blurred vision
- Seizures
- Coma
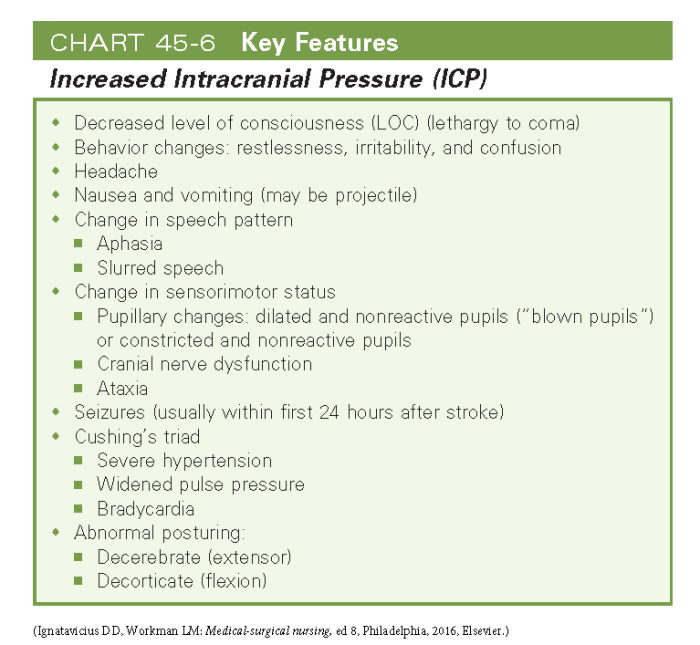
Clinical Manifestations of Increased Intracranial Pressure, Nursing diagnosis increased intracranial pressure
The clinical manifestations of increased ICP vary depending on the severity of the pressure increase. Mild increases in ICP may cause only subtle symptoms, such as headache or nausea. More severe increases in ICP can lead to more serious symptoms, such as seizures or coma.
Nurses play a vital role in assessing and monitoring patients for signs and symptoms of increased ICP. Early detection and intervention are essential to prevent serious complications.
The following are some of the common signs and symptoms of increased ICP:
- Headache
- Nausea and vomiting
- Blurred vision
- Seizures
- Coma
In addition to these signs and symptoms, nurses should also monitor the patient’s vital signs and neurological status. Changes in vital signs, such as blood pressure and heart rate, can be indicative of increased ICP. Neurological changes, such as decreased level of consciousness or pupillary changes, can also be indicative of increased ICP.
Nursing Assessment and Management of Increased Intracranial Pressure
Nurses play a vital role in the assessment and management of increased ICP. The following are some of the key nursing assessment strategies:
- Monitor the patient’s vital signs and neurological status.
- Assess the patient’s level of consciousness using the Glasgow Coma Scale (GCS).
- Assess the patient’s pupillary response.
- Assess the patient’s head circumference.
- Assess the patient’s skin for signs of edema.
The following are some of the key nursing interventions for managing increased ICP:
- Positioning and head elevation: Elevating the patient’s head promotes venous drainage from the brain and helps to reduce ICP.
- Fluid management: Fluid restriction is often used to reduce the amount of CSF in the ventricles and help to reduce ICP.
- Sedation and analgesia: Sedation and analgesia can be used to reduce the patient’s agitation and pain, which can help to reduce ICP.
- Osmotic agents: Osmotic agents, such as mannitol and glycerol, can be used to draw fluid out of the brain and help to reduce ICP.
Collaborative Management of Increased Intracranial Pressure
The management of increased ICP is a collaborative effort between nurses, physicians, and other healthcare professionals. The following are some of the key collaborative management strategies:
- Surgical interventions: Surgical interventions, such as craniotomy or ventriculostomy, may be necessary to relieve increased ICP.
- Monitoring ICP: ICP monitoring is used to measure the pressure within the cranial vault. This information can be used to guide treatment and assess the patient’s response to therapy.
- Post-operative care: After surgical intervention, the patient will need to be closely monitored for signs and symptoms of increased ICP.
Education and Support for Patients and Families
Patients and families need to be educated about the signs and symptoms of increased ICP. They also need to be aware of the importance of monitoring for these signs and symptoms and seeking medical attention if they occur.
Nurses can provide education and support to patients and families by:
- Teaching patients and families about the signs and symptoms of increased ICP.
- Explaining the importance of monitoring for these signs and symptoms.
- Providing information about the treatment options for increased ICP.
- Offering support and resources to patients and families.
FAQ Overview: Nursing Diagnosis Increased Intracranial Pressure
What are the common causes of increased intracranial pressure?
Increased intracranial pressure can result from various factors, including head injuries, stroke, brain tumors, infections, and bleeding within the skull.
How is increased intracranial pressure diagnosed?
Diagnosis involves a combination of physical examination, neurological assessment, and imaging techniques such as CT scans or MRIs to visualize the brain and assess ICP levels.
What are the nursing interventions for managing increased intracranial pressure?
Nursing interventions focus on reducing ICP and preventing complications. They include positioning the patient to promote venous drainage, administering fluids and medications to control ICP, and providing sedation and analgesia for comfort.
Why is interdisciplinary collaboration crucial in managing increased intracranial pressure?
Effective management requires collaboration among nurses, physicians, neurologists, and other healthcare professionals to provide comprehensive care, monitor ICP, and address complications promptly.
How can patient and family education improve outcomes in increased intracranial pressure?
Educating patients and families about the condition, signs and symptoms to monitor, and the importance of adhering to treatment plans empowers them to participate actively in their care and promotes better outcomes.